According to American Society of Clinical Oncology, there is an estimated 53,260 adults (38,330 men and 14,880 women) in the United States will be diagnosed with oral and oropharyngeal cancer in the year 2020. Rates of these cancers are more than twice as high in men as in women. Oral and oropharyngeal cancer are the eighth most common cancer among men. The average age of diagnosis is 62. About 25% of cases occur in people younger than 55, but these cancers are rare in children.

Persistent human papillomavirus (HPV) infection is now the leading cause of cancers in the oropharynx (tonsils and tongue base area of the throat). In what is believed to be a world-first, a simple saliva test developed by Queensland University of Technology (QUT) biomedical scientists has detected early throat cancer in a person who had no symptom and no clinical signs of cancer.
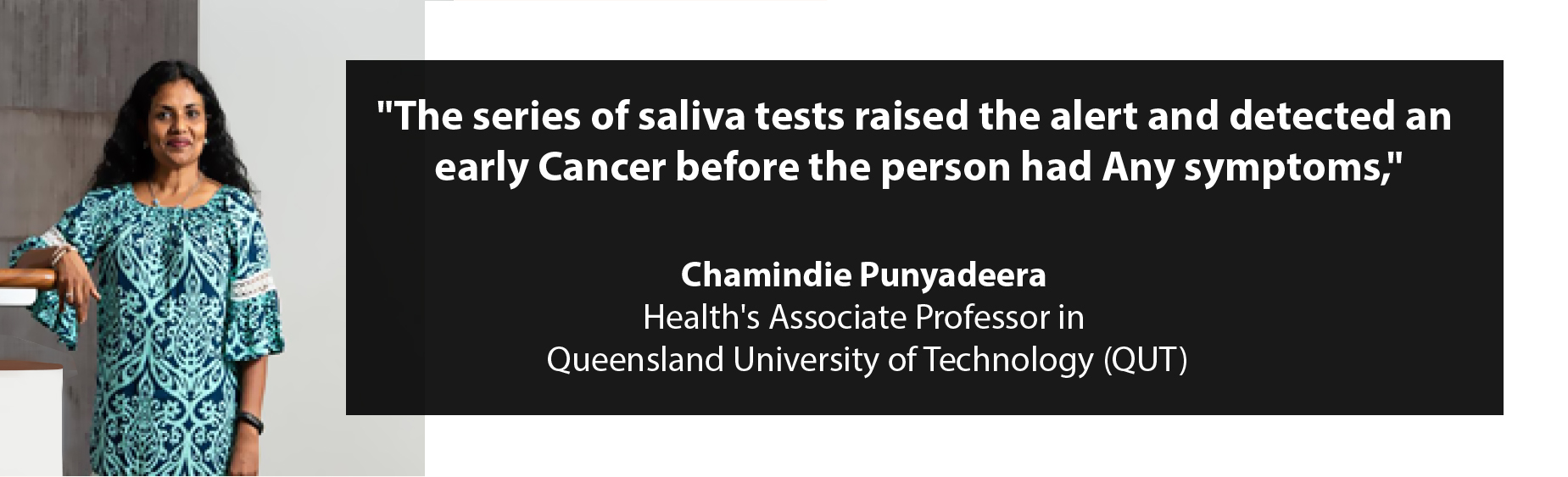
“The series of saliva tests raised the alert and detected an early cancer before the person had any symptoms,” said QUT Faculty of Health’s Associate Professor Chamindie Punyadeera, who, with Dr Kai Tang, developed the test. Professor Punyadeera said the discovery was made during an HPV-prevalence study which included 665 healthy individuals. The incidence of high-risk human papillomavirus (HPV)-driven throat cancers is on the rise in developed countries. Unfortunately, it is often discovered only when it is more advanced, with patients needing complicated and highly impactful treatment options. In the US, HPV-driven throat cancers have surpassed cervical cancers as the most common cancer caused by HPV. However, unlike cervical cancer, up until now, there has been no screening test for this type of oropharyngeal cancer.
 “To take the test, all the person has to do is give a salivary
oral rinse sample. When the test shows HPV-16 DNA, it is repeated and if
the presence of HPV-16 is persistent over a period of time we would
“To take the test, all the person has to do is give a salivary
oral rinse sample. When the test shows HPV-16 DNA, it is repeated and if
the presence of HPV-16 is persistent over a period of time we wouldbe suspicious that there may be underlying cancer. “The person whom we reported in this study had been consistently HPV-16 DNA positive for 36 months, with a steadily rising count of HPV-16 DNA after testing at 6, 12 and 36 months. The patient was found to have a 2mm squamous cell carcinoma in the left tonsil, treated by tonsillectomy. This has given our patient a high chance of cure with very straightforward treatment. Since the surgery, the patient has had no evidence of HPV-16 DNA in his saliva.”
The presence of this pattern of elevated salivary HPV-DNA must be fully evaluated, as it may provide the critical marker for early cancer detection. Professor Punyadeera said this was the first-ever case of histologically confirmed diagnosis of an asymptomatic, hidden throat cancer, diagnosed with a saliva screening test and that wider validation studies are required to confirm this finding.
REFERENCE
1. American Society of Clinical Oncology (2020). Oral and oropharyngeal cancer statistics. Retrieved from
https://www.cancer.net/cancer-types/oral-and-oropharyngeal-cancer/statistics
2. Higuera, V. (2018, August 9).What is throat cancer?. Heartline. Retrieved May 14, 2020 from
https://www.healthline.com/health/cancer-throat-or-larynx
3. Queensland University of Technology. (2020, May 12). World-first saliva test detects hidden throat cancer. ScienceDaily. Retrieved May 14, 2020 from www.sciencedaily.com/releases/2020/05/200512093950.htm
4. Queensland University of Technology. (2020, May 12).World-first saliva test detects hidden throat cancer. Medicalxpress. Retrieved May 14, 2020 from
https://medicalxpress.com/news/2020-05-world-first-saliva-hidden-throat-cancer.html
IMAGE GLOSSARY
-
https://www.google.com/url?sa=i&url=https%3A%2F%2Fwwwdocwirenews.com%2Fdocwire-pick%2Fhem-onc-picks%2Fscientists-develop-first-saliva-test-that-detects-throat-cancer-in-asymptomatic-patients%2F&psig=AOvVaw3KPDYoCgZS-H2xpkfLidUe&ust=1589956569970000&source=images&cd=vfe&ved=0CAIQjRxqFwoTCOix3bmtv-kCFQAAAAAdAAAAABAV -
https://www.google.com/url?sa=i&url=https%3A%2F%2Ftwitter.com%2FQUT%2Fstatus%2F1144020919498596352&psig=AOvVaw381qzzqMwZ3Qatq1DBEFxG&ust=1589953762276000&source=images&cd=vfe&ved=0CAIQjRxqFwoTCKC55PCtv-kCFQAAAAAdAAAAABAD -
https://www.google.com/url?sa=i&url=https%3A%2F%2Fwww.qut.edu.au%2Fresearch%2Farticle%3Fid%3D144469&psig=AOvVaw09oZ1bVIxrHd3pIdaHfuHv&ust=1589957292759000&source=images&cd=vfe&ved=0CAIQjRxqFwoTCODQ0dqqv-kCFQAAAAAdAAAAABAa


 real benefit to patients if the connection between the patient and the prosthesis is safe and reliable in the long term. Our results are the product of many years of work, and now we can Finally present the first bionic arm prosthesis that can be reliably controlled using implanted electrodes, while also conveying sensations to the user in everyday life,” continues Prof. Catalan. Since receiving prostheses, the patients have used them daily in all their professional and personal activities.
real benefit to patients if the connection between the patient and the prosthesis is safe and reliable in the long term. Our results are the product of many years of work, and now we can Finally present the first bionic arm prosthesis that can be reliably controlled using implanted electrodes, while also conveying sensations to the user in everyday life,” continues Prof. Catalan. Since receiving prostheses, the patients have used them daily in all their professional and personal activities.


 “Our goal is to get information out to the community and to
“Our goal is to get information out to the community and to
